Managing Burnout — Part Two: Social Determinants of Health
In today’s blog, Part 2 of this Burnout series, I will share insights into how the Social Determinants of Health impact burnout and our wellbeing, as well as how employers can make a difference.
In the last part of this series, I will explore the broader Organizational Determinants of Burnout and share some evidence-based tips for leaders and organizations.
In my last blog, Part 1 of this 3 part Burnout series, I shared insights around the mechanism of burnout and strategies that you can do personally to improve your risk for burnout. I mentioned, that I use three large groupings to better understand the various factors that put one at risk and approaches to reduce or mitigate this risk. To recount these are :
- PDOH: Personal Determinants of Health
- SDOH: Social Determinants of Health
- ODOH: Organizational Determinants of Health
In today’s blog, I will focus on the Social Determinants of Health and their impact on burnout and mental well-being.
The World Health Organization defines mental health as a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community.
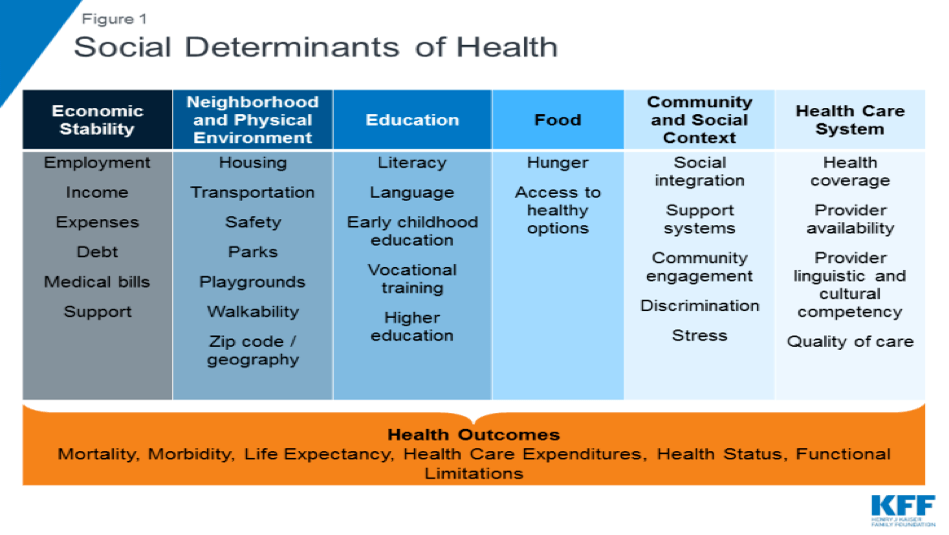
If we want to create a mentally healthy work environment for all employees, we need to understand what determines health. Eighty to Ninety percent of what drives our health throughout a lifetime is our social and physical environment. These are known as the “social determinants of health” — conditions in the environments where people live, play, learn, and work that may influence a person’s ability to manage their health or cope with stress.
In recent years, a growing body of evidence shows the critical role of these determinants for mental health outcomes such as anxiety, stress, burnout and depression.
The long-term effects of adverse psychosocial events have become better understood in recent decades. Socioeconomic status is linked to physical and mental health and to the costs associated with mental health-related disability, lost economic productivity, and psychiatric care. This linkage highlights the role of the social determinants of mental health as a vector for reducing the burden of psychiatric disease.
Addressing these unmet essential needs is important for improving health and reducing health disparities. Moreover, the allostatic load and ongoing stress caused by these unmet needs can amplify or accelerate the development of burnout.
The implementation of evidence-based interventions to reduce the impact of harmful psychosocial factors at a population level has the potential to alter the course of burnout and other mental ill health as a form of primary prevention.
While many of these factors are beyond our control or an employer’s control, understanding their impact can help you build empathy to not only understand the needs of friends, family or colleagues but to help support them. It also helps leaders and managers build empathy and trust through a greater understanding of the needs of their team with an aim to support and develop strategies and solutions that meet those needs.
During 2021, the Kaiser Foundation reported in a representative sample of US adults:
ADULTS EXPERIENCE with SDOH HARDSHIPS – 2021
- 16% reported that they or someone in their household had experienced a loss of income in the past four weeks
- 52% reported difficult paying for usual household expenses in the past seven days
- 30% used credit cards or loans to meet household spending needs
- 7% had no confidence in their ability to make next month’s housing payment (across renters and owners)
- 9% reported food insufficiency in their household
- 32% reported symptoms of depression or anxiety
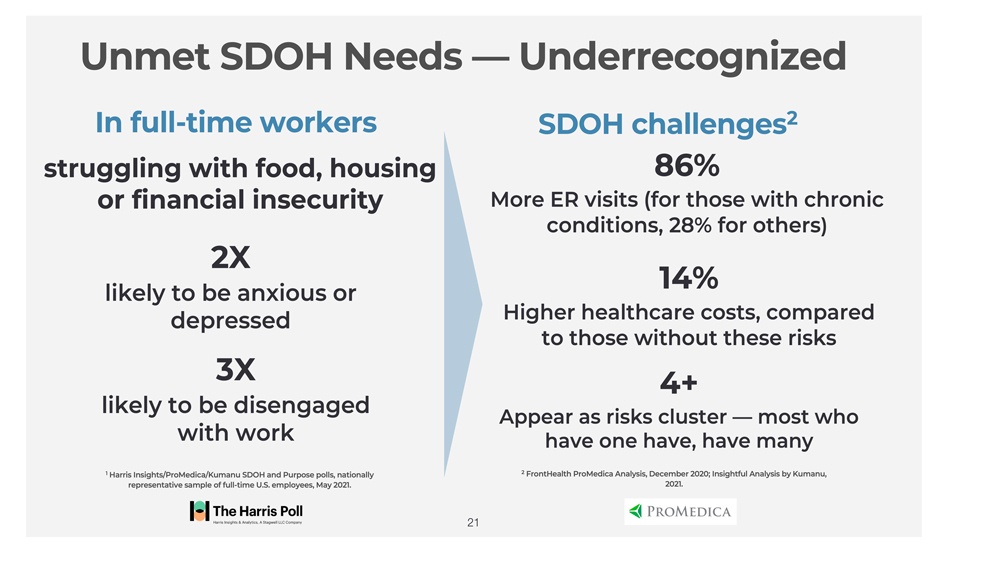
While we often think these risks are confined to the poor or more disadvantaged parts of our society, Kumanu working with the Harris group and ProMedica National Social Determinants of Health Institute uncovered surprising findings that suggest these challenges are far more prevalent amongst the full-time workforce than previously known.
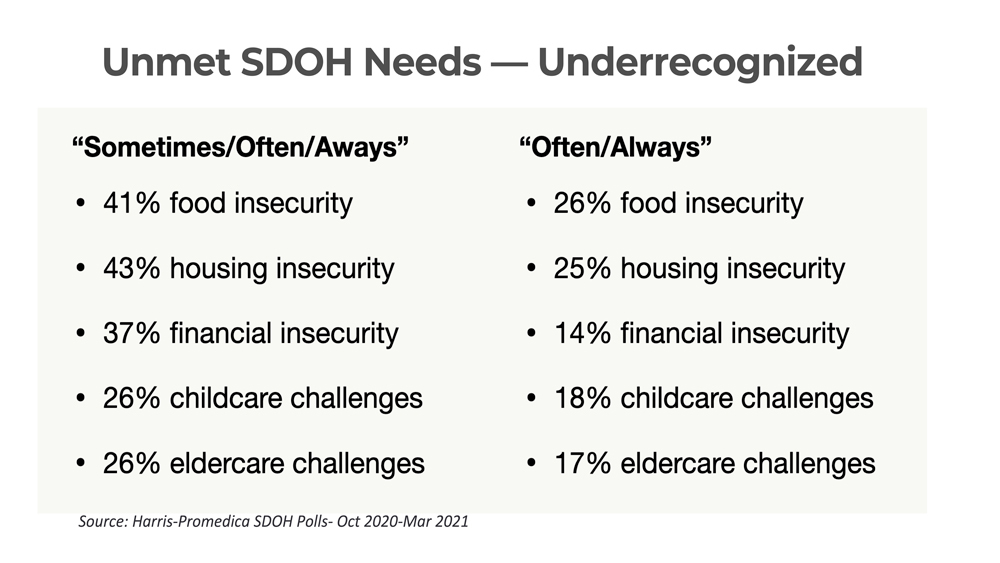
These unmet essential needs have a direct and negative impact on the employer. Employees struggling with these challenges are more distracted, less engaged and less productive. These added stressors impact existing health conditions and increase the risk for burnout leading to more ER visits, higher healthcare costs, and increased risk for mental ill health. While most employers offer health insurance coverage and well-being programs these may not be enough for employees who are struggling with putting food on the table or having a difficult time making it to work due to transportation and caregiver challenges.
Employers are well positioned to make a difference as they have routine, frequent contact with their employees, determine what benefits employees can receive, and can access information that may point to social needs affecting employee health, well-being and productivity at work. The resources are available, but the mechanism to connect those in need, in the right moment to either community or organizational resources is often lacking.
Fortunately, innovative digital solutions can not only identify these unmet essential needs, but can connect those in need to relevant services and resources and most importantly, help activate their use through greater agency and improvements in overall resilience and mental wellbeing.
How would this work in practice? A technology solution available 24/7 can help:
- Set the stage and de-stigmatize the topic of social determinants of health barriers through communication channels
- Identify social determinants risks through a confidential user assessment feature with immediate personalized feedback
- Offer personalized resources, tailored suggestions and linkage to health system resources, community resources, and 1:1 interventions
- Follow-up via automated surveys and updates to gauge actions, measure impacts, and offer ongoing follow-on support
- Measures changes over time on user health, engagement, and quality of life providing benchmarks and comparison data at individual and population level — driving better decision-making and population insights
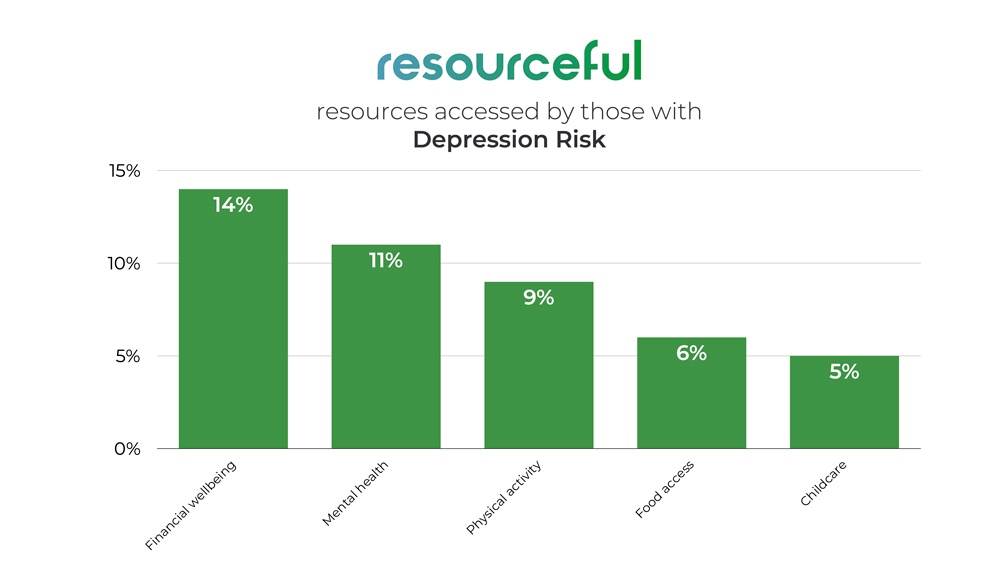
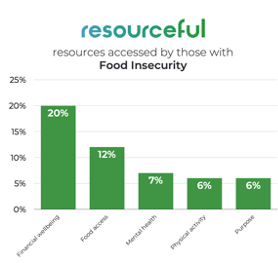
We also see that one unmet need can be associated with other essential needs not met as well as physical and mental health needs.
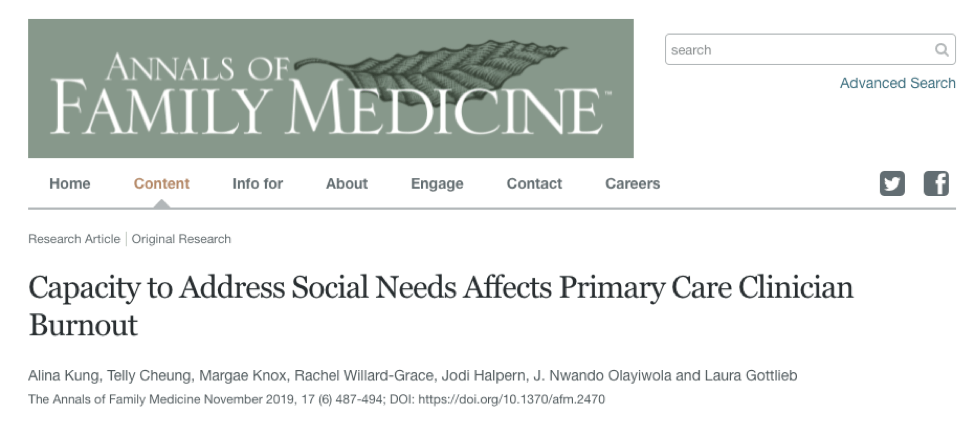
For industries of ‘caregivers’ such as the healthcare industry, tackling patients’ social needs may reduce clinician burnout. Clinician Burnout can result from any number of systemic factors. For some, it’s administrative burden in its many forms, compassion fatigue or loss of self-efficacy or ability to make a difference such as the inability to connect patients with the resources they need beyond the exam room, such as adequate food and a safe place to stay. Over time, not being able to address the social needs of patients can wear away at even the most resilient health care professional. A study examined the relationship between burnout in primary care clinicians and the capacity of primary care clinics to address patients’ social needs. They found clear associations between the inability to meet social needs and burnout levels, they also found that increasing services that address social needs in the clinic appeared to mitigate burnout symptoms and improve clinician morale.
Be an empathetic leader
Employee needs connected to these factors are greater than ever in this moment, and aren’t limited to the lowest wage workers. For employers, the goal should be to understand and be sensitive to these other factors—and then build support that addresses common needs and makes the workplace a positive catalyst for mental health. A leaders’ ability to listen and respond with empathy is highly correlated with their employee’s engagement, retention and overall performance. In fact, research based on an analysis of companies that focus on empathy within the organization, as well as on customers, find that these companies have significantly higher performance on average.
The outcome can be employees that thrive versus survive. The scope of worksite wellbeing initiatives today extends beyond individuals’ physical health to now include Social Determinants of Health.
Through internal collaboration and external partnerships that address social risk factors and employees’ needs, employers can develop a healthy, high-performing workforce.
The good news is there is much employers can do!
Stay tuned for my next blog, the last in this 3 part series. I will go into more detail on the Organizational Determinants of Health — the culture, team dynamics, norms and leadership behaviors that can either add to or improve burnout risk.
About the Author
Robert Carr, MD, MPH, FACPM
Chief Medical Officer
Robert Carr was most recently Senior Vice President & Corporate Medical Director at GlaxoSmithKline and on the faculty at Georgetown University. He received his Doctor of Medicine from the University of Miami School of Medicine and his Masters of Public Health and Preventive Medicine Residency from the John Hopkins Bloomberg School of Hygiene and Public Health. Bob also served as the President of the American College of Preventive Medicine
Stay on top of the news
Subscribe today and receive our Reimagining Wellbeing newsletter delivered to your inbox every month!